As an Amazon affiliate, I may earn from qualifying purchases. Please read our Disclaimer and Privacy Policy.
If you’re asking the question, “How long do hospice patients live without eating?” there’s a good chance your loved one is approaching the final stage of life.
It’s a challenging time, but also a time of learning and acceptance.
I’ve been in this position with my mother. Like you, I wanted to know how much longer she had to live.
She had stopped eating and drinking, slept more often than not, and her facial muscles had relaxed so much that her mouth hung open.
While family members helped with her care as much as possible, it was the palliative care medical professionals who made sure mom was as comfortable as she could be.

They were open and honest about what was happening and, to be honest, she never appeared to be suffering.
They told me not to force my mother to eat or drink if she didn’t want to. As you’ll see further into this post, there are very good reasons for this.
In this post, I’ll use the experience I had with my mother’s last days, including everything I learned about terminal dehydration and end of life anorexia (not related to an eating disorder). I’ll also explain why intravenous fluids, feeding tubes, and force feeding can increase suffering in a dying person.
How long do hospice patients live without eating?
According to Vitas Healthcare, patients can die in as early as a few days without food and water.
Typically, a person can survive without food for about 1 to 3 weeks, depending on their health and hydration levels. If the hospice patient is still drinking fluids, they may survive longer.
Signs of approaching death include decreased appetitie, physical changes, changes in hydration needs, changed in food intake.
Factors That Influence Survival Time
According to Healthline, the maximum time the body can survive without food or water is thought to be about one week.
However, as long as the person is staying hydrated with water, survival time could extend upwards of 2 to 3 months.
From my experience, my mother (a cancer patient) survived a little over 2 months with only water.
The length of time hospice patients live without eating is an estimate because every case is different. The following factors can play a role in the outcomes:
Hydration
A patient who is still consuming liquids may live longer than one who has stopped both eating and drinking.
Overall health condition
If a patient’s organs are already failing, they may pass away more quickly.
Medication and comfort care
Hospice care teams provide medication to manage symptoms, which can also play a role in extending or shortening life expectancy.

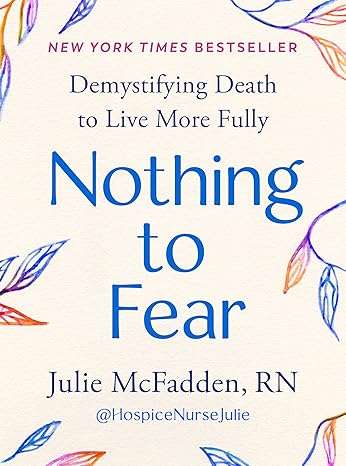
Nothing to Fear: Demystifying Death to Live More Fully
Julie McFadden is a hospice nurse with a huge TikTok following, and for good reason. The love and care she extends to her patients, and their families, is something to see. She’s a wealth of information about the dying person and has, quite literally, seen it all.
I highly recommend her book, Nothing to Fear, seen below.
As Julie says, the body knows how to die. The more you interrupt that process with unnecessary medical interventions, the worse off your loved one will be.
Read Julie’s NEW YORK TIMES BEST SELLER: Nothing to Fear, Demystifying Death to Live More Fully.
Nothing to Fear
Julie explains it best
Watch the following video as Julie describes the benefits of not providing IV fluids or food to a dying patient.
Why Do Hospice Patients Stop Eating?
There are several reasons why a hospice patient may no longer want to eat:
Loss of appetite
As organs begin to fail, the body no longer signals hunger in the same way. The decrease of appetite and thirst is not painful and is an expected part of dying.
As the end-of-life process progresses, it’s common for a person’s fluid intake and food consumption to significantly reduce. This is a natural response of the body as it prepares to shut down.
Difficulty swallowing
Dysphagia, or difficulty swallowing, is common among patients nearing the end of life.
Fatigue and weakness
Many hospice patients are too tired or weak to consume food.
The natural part of the dying process often includes physical changes such as shortness of breath and a decreased sense of hunger or thirst.
I feel like I’m starving my loved one!
It’s normal and common for people to want to nourish their loved one in their last days. However, it’s important to understand that forcing fluids and food at this point can make things significantly worse for your loved one.
It’s okay to stop nutrition and hydration as your loved one approaches death.
How long do hospice patients live without eating? According to Crossroads Hospital & Palliative Care, patients can live for varying lengths of time without eating. The range is from a few days to several weeks.
Ultimately, every person is unique. There may be variables, as mentioned earlier, that can affect the length of time a hospice patient can live without eating.
Artificial Nutrition
It’s hard to watch a loved one die. We intuitively want to do whatever we can to reduce their suffering. The fact is, decreasing food and fluid intake is a natural part of the process.
As death approaches, most dying people don’t feel thirst or hunger. Unfortunately, providing food and fluids by artificial means can increase uncomfortable symptoms like shortness of breath, respiratory congestion, restlessness, nausea, and vomiting.
Tube Feeding (nasogastric tube)
According to the Palliative Care Network of Wisconsin, tube feeding may not be the best approach for a dying patient. For example, observational studies have shown a high incidence of aspiration pneumonia in hospice patients who have been tube fed.
Since most actively dying patients do not experience hunger or thirst, tube feeding seems counterintuitive to the dying process.
Read: Tube Feed or Not Tube Feed?
Force Feeding
It’s important not to force food into a hospice patient. The person is likely unable to swallow effectively and can choke or aspirate on food.
Forced feeding can also cause other problems including:
- nausea
- vomiting
- abdominal bloating
- excessive gas
- constipation
- diarrhea
Deciding whether to have a feeding tube
Watch this video from Nurse Julie on whether a feeding tube is appropriate.
You’re doing just fine!
It sounds strange to say, but forcing the person to eat and drink will not bring comfort to the person’s final days.
My mother’s nurse explained to me that end-of-life patients go through a natural, normal dying process. The body knows how to die and begins to shut down signals to the body that would indicate appetite or thirst.
When someone is at the end of life, their organs are shutting down and not working the way they should be.
The body’s biological systems are programmed to gradually shut down as part of the dying process. Reduced food and water intake is a sign that the body is transitioning to its final stage.
Is it dementia?
There are a number of terminal illnesses and each one requires unique end of life care. Dementia has an added layer of difficulty as communication becomes more difficult.
If you are in this situation, or know someone who is, read: 7 Things Not to Say to Someone With Dementia

The Role of Hospice in End-of-Life Care
When a hospice patient stops eating, the hospice care team shifts its focus from curative treatments to comfort and quality of life.
The goal is not to prolong life but to ensure the patient’s remaining days are as peaceful and pain-free as possible.
Symptom management:
Hospice teams provide medications for pain, nausea, or other symptoms related to stopping food intake.
Emotional and spiritual support
Hospice care includes counseling and spiritual services for both the patient and their loved ones during this difficult time.
If you are ever worried about something related to your loved one, don’t hesitate to ask the hospice team for guidance.
They are there to provide comfort and guidance during this time, helping to ensure that loved ones understand these changes and providing the best way to offer support.
Education and guidance
Caregivers are often unsure how long hospice patients live without eating and what to expect. Hospice professionals offer valuable information to help families prepare.
Other types of healthcare support
When my mother was in her final days, the family brought in a home healthcare worker to wash my mother. She wasn’t able to get up to get into the tub or shower and had to be sponge-bathed daily.
If you’re reading this, and have questions about showering and the elderly, read: How Often Should The Elderly Shower For Their Health.
Is it Painful for Hospice Patients to Stop Eating?
It’s natural to worry that a loved one may suffer if they stop eating, but the body adapts to this process.
As the body shuts down, it no longer requires the energy that food provides, and most patients do not experience hunger.
Hospice care teams ensure that patients are comfortable, using medications to address any discomfort or distress that may arise.
What to Expect When a Hospice Patient Stops Eating
When a hospice patient stops eating and drinking, there are certain signs that indicate death is approaching.
These include:
Increased sleepiness or unconsciousness
The patient may spend more time asleep and less time awake.
Changes in breathing
Breathing may become irregular or shallow.
Cool extremities
Hands and feet may become cold as circulation slows down.
These changes are natural and part of the body’s way of preparing for death. If you’re concerned about your loved one’s comfort, talk to a hospice nurse.

Conclusion
Understanding how long hospice patients live without eating is a challenging but important part of preparing for the end-of-life experience.
While most hospice patients live for about one to two weeks after they stop eating, the actual timeline can vary based on individual health factors.
Hospice care teams play a crucial role in ensuring patients are comfortable, while also providing support and guidance for their families during this time.
Remember, every end-of-life journey is unique, and the focus should always be on comfort and quality of life rather than trying to predict exact timelines.
If you or a loved one are navigating this difficult journey, hospice professionals are there to offer the compassionate care and support needed for both patients and families.



